Mental health records missing from RI’s gun background check data
Buying a gun from a dealer – say, a sporting goods store – triggers a federal background check. If you’re a convicted felon, you would fail the background check. So, too, if you’ve been involuntarily committed to an institution or otherwise ruled mentally ill. But the federal database against which background checks are run is only as good as the data. And Rhode Island is one of only four states that haven’t submitted any mental health records at all, according to a recent report out from a group called Mayors Against Illegal Guns. The New York Times ran a story about it here, too.
So why hasn’t Rhode Island complied with federal law? In short, the report explains, it’s complicated. For starters, it’s not clear to some state officials which kinds of mental health records should be shared. Then there are the varying interpretations of HIPAA, or privacy laws, about sharing someone’s health information (including substance abuse-related convictions and treatment). Lack of funding is another reason.
Humbly, I propose another reason: a deep misgiving, perhaps, about the implications of sharing this kind of information. Consider: if you were convicted of a substance abuse-related offense 15 years ago, but have been in recovery ever since, should you be allowed to buy a gun? If you were committed to an institution eight years ago but have since been treated, successfully, for bipolar disorder with medication, should you be allowed to buy a gun? I won’t attempt to answer those questions, but I invite comments. All I can say is: murky waters.
So what’s happening now in Rhode Island? Here’s what the report finds about efforts to address the issue here, based on confidential interviews with state officials (emphasis mine):
…a state official reported that the state is actively working to get records in. Representatives from the Rhode Island Law Enforcement Telecommunications System, the state attorney general, the state courts, and others held a summit to discuss record sharing, and state officials recently attended a regional NICS conference in Connecticut to determine how to overcome Rhode Island’s funding, logistical, and privacy obstacles. The state’s primary problem is a lack of funding to update software or implement record sharing. Rhode Island does not have a gun rights restoration program and is thus currently ineligible for federal NARIP grants. The NICS legal team is actively helping Rhode Island to draft laws. Privacy does not appear to be a major problem, but a state official believes that HIPAA privacy laws will be a hurdle for some civil commitment files. State officials are also apparently unsure of exactly which mental health records must be gathered for NICS submission, though the official interviewed by Mayors Against Illegal Guns contends that record submission should move swiftly once that is clarified and the software is in place, especially because Rhode Island mental health records are already kept in electronic form.
More public health research into gun violence?
We’re all still reeling from the Newtown, CT tragedy. Reeling…and trying to make sense of what happened and why. And that’s where health care professionals and scientists are often able to help. We’ve got some of the best right here in Rhode Island, who would probably love to be able to answer questions like: Could we get better at predicting who is likely to commit a crime with a gun? Does having access to a gun in the house make you more likely to commit a crime with a gun?
But here’s the thing. We don’t really know. And it’s not exactly their fault.
A new editorial today in the Journal of the American Medical Association lays out how researchers’ efforts to understand the why and how of gun violence have been stymied by politics. It also lays out how such research could give us a better understanding of this kind of violence. We’ve done quite a bit of work, the authors say, on what leads people to be violent. But we don’t know as much about “how easy access to firearms mitigates or amplifies both the likelihood and consequences of these acts.” Here’s why:
The nation might be in a better position to act if medical and public health researchers had continued to study these issues as diligently as some of us did between 1985 and 1997. But in 1996, pro-gun members of Congress mounted an all-out effort to eliminate the National Center for Injury Prevention and Control at the Centers for Disease Control and Prevention (CDC). Although they failed to defund the center, the House of Representatives removed $2.6 million from the CDC’s budget—precisely the amount the agency had spent on firearm injury research the previous year. Funding was restored in joint conference committee, but the money was earmarked for traumatic brain injury. The effect was sharply reduced support for firearm injury research.
The authors – a doctor from the RAND corporation in Washington, D.C. and another from Seattle Children’s Hospital – point out a number of other ways health care workers and researchers have been silenced on gun issues. In Florida, doctors may not be able to discuss or make notes about firearm safety at all, if some legislation passes. And then there’s the difficulty of tracking down gun data to produce meaningful statistics. But it’s this kind of public health research that’s led to the reduction of harm from other kinds of threats, as in the case of public seat belt awareness campaigns based on motor vehicle crash research.
Perhaps things are about to change.
Interview: RI Hospital ER chief: “There has to be a better way.”
This week, I’ve been covering Rhode Island’s efforts to change the way we deal with substance abusers who frequent the emergency room (part 1, part 2). I talked to emergency dispatchers, firefighters, addiction treatment specialists, public officials, and more. And I visited an alternative to the ER, a so-called “wet shelter” or sobering center in Cambridge, MA to see how that’s helping reduce ER visits.
Emergency room doctors are also on the front lines in this story, and that’s why I’m glad I got the chance to talk to Dr. Brian Zink, head of emergency medicine at Rhode Island and Miriam Hospitals. I’ve included the full interview, below, which you can listen to right on this page or download for later.
Every sizable city, says Zink, has a population of alcoholics and drug addicts whose addiction has gotten so bad they’re on the street and, often, quite ill. Providence is no different. An ambulance is called, the intoxicated person is brought to the emergency department, and doctors and nurses there are obligated to care for them until they sober up. They get spit on, there are fights, patients urinate on the floor. It can be frustrating, says Zink, for staff, mostly because they know it isn’t the best place to care for patients. But Zink and his colleagues decided to do something about it. They formed a coalition called “Closing the Addiction Treatment Gap,” got Rhode Island lawmakers’ attention, and are now helping formulate a plan to open a sobering center in Providence. The idea is to move people who simply need to sober up out of the emergency room, to a place where they can be offered substance abuse treatment and other resources, like housing. That, says Zink, would not only mean that addicts get more appropriate treatment. It would save money and free up beds:
“At any one time, we’ll have probably six to 15 of our precious treatment spots occupied by people who are simply drunk or under the effects of drugs and just sobering up, basically…. If you look at a Friday night or Saturday night…. we might have 20 to 25 beds with alcohol-intoxicated people.”
Learn more about the perspective of ER doctors, the impact of “frequent fliers” on the ER, and why now is the right time for change in this interview with Dr. Brian Zink.
RI submits health insurance exchange “blueprint”
The Ocean State has sent the federal government – ahead of schedule – what it’s calling a “blueprint” for the state’s health benefits exchange. The blueprint is a collection of draft documents, the exchange’s creators say, that reflect the state’s best thinking to-date on how the exchange should work. Its submission is a key milestone for states developing their own exchanges.
The exchange, a key part of the Affordable Care Act, will be an online portal for all Rhode Islanders looking for a health insurance plan. It will be the place where Rhode Islanders who can’t afford health insurance will find not only a plan but access to a government subsidy to help pay for it.
And, of course, there’s more to it than that. See my earlier post about the exchange here. But also, see this Blueprint Executive Summary, released yesterday by the exchange’s advisory board. It’s got a great description of what they’ve submitted to the federal government so far, what the exchange will be designed to do, and how it will affect you (as well as how you can participate by providing input).
Sen. Whitehouse: spare Medicare, reform the system
Sen. Sheldon Whitehouse (D-R.I.) published an op-ed on Politico Tuesday urging President Obama not to agree to any Medicare cuts in the fiscal cliff negotiations. The reason: reforming the health care system, including the way we deliver and pay for health care, will add up to all the savings we need.
Whitehouse writes:
…the Affordable Care Act contains many of the tools we need to achieve our goals — tools like better coordinating care between primary physicians and specialists, paying for quality of care rather than quantity of care, reducing medical errors and hospital acquired infections, replacing paper health records with electronic records and more.
Give it a read, and let me know what you think. Whether or not you agree with the senator that we can bring down health care costs without cutting Medicare, my own reporting confirms that he’s right about this: it’s tough to quantify, up front, how much each particular change in the system will save, and when. Sometimes it takes a while before you see savings, and you might be saving in ways you never anticipated.
Update: Rhode Island’s Health Benefits Exchange
Perhaps you’ve been wondering where things stand with Rhode Island’s efforts to build its own online health insurance marketplace?
Wonder no more! I joined our All Things Considered host Dave Fallon in the studio yesterday to give an update on the exchange. That’s because I got the chance to catch up with Christy Ferguson, who heads the group that’s planning and developing the exchange, and wanted to share what I learned.
Here’s a link to listen to that conversation.
Here are a few key takeaways if you don’t have time to listen:
- The exchange will operate as kind of a gateway for Rhode Islanders seeking health insurance, in particular those who don’t have any, can’t afford it, or whose small employer has given them the flexibility to seek a health plan on their own.
- It should be up and running – meaning you can sign up – by November 2013.
- The exchange’s developers are negotiating with Rhode Island’s four major health plan providers to develop a variety of plans that meet Rhode Islanders’ range of needs and budgets.
- I’m told that, ultimately, the exchange will provide Rhode Islanders with more flexibility when choosing a health plan.
By 2025, 25% more primary care docs needed
A new study in the Annals of Family Medicine projects the country will need about 52,000 more primary care doctors by 2025. The study’s authors calculated that we currently have about 206,000.They based their projections on the number of patients primary care docs currently see in office visits per year, and how many might be expected based on how much our population is set to grow, how much more an aging population will need primary care, and how many people will have access to a primary care doctor for the first time as a result of the Affordable Care Act.
The studies authors, however, acknowledge that their projects don’t take into account the roles that nurse practitioners and physician assistants play in providing primary care. In my own experience, that role has been huge. But it’s one of many reports to sound the alarm: we don’t have enough doctors engaged in direct patient primary care to meet the needs of a growing, aging, and newly-insured population.
Read it here.
So what’s to be done? Does the burden rest solely on graduate medical education programs and enticing doctors-to-be to enter primary care? Some would say that part of the solution has to be in realigning the way we compensate doctors, that rather than paying per service, we pay them for healthy outcomes. The way things work now, primary care doctors simply earn less, and, to some bright, young medical students considering a future clouded by debt, that might not look like the smartest path to follow.
(Shameless plug! You can read more about the experiences of future doctors, by the way, on our Future Docs blog.)
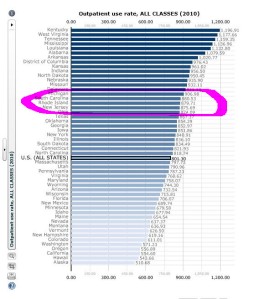
RI has highest antibiotic use in New England
And that matters to you because….? Well, because if the bacterial infection you’re suffering from has evolved a resistance to available antibiotics, it will be harder to treat. There’s some new data about the spread of resistance, and new attention on it today.
The CDC is promoting its “Get Smart About Antibiotics Week,” and the Center for Disease Dynamics, Economics, and Policy has just updated its “ResistanceMap,” which shows where the resistance hot spots are in the U.S. and internationally.
(About the graphic: this is a smallish screenshot of the CDDEP’s state-by-state resistance data on which I’ve circled Rhode Island. Click on it for a larger view. And you can see the original here.)
Here’s some background on the problem from the CDDEP:
Scientists have been aware of antibiotic resistance since shortly after the discovery of penicillin, western medicine’s first antibiotic. To a certain extent resistance is inevitable—as we use an antibiotic over time, resistance to the drug gradually evolves, making infections more difficult to treat and necessitating new and more powerful drugs. However, the development of resistance is also impacted by our actions—for example by how often we prescribe and use antibiotics, and how well we control and prevent infections acquired in the hospital. In order to design sensible solutions that prolong the useful life of antibiotics, policymakers need to be able to provide factual evidence, identify trends and measure the scope of the resistance problem.